Emerging Evidence Supports the Hypothesis that Neutrophil Extracellular Traps are a Major Factor in Genesis and Progression of Chronic Obstructive Pulmonary Disease
Astrid Obermayer1*, Walter Stoiber1, Fikreta Grabcanovic-Musija2, Michael Studnicka2
1Department of Biosciences, Biomedical Ultrastructure Research, University of Salzburg, Salzburg, Austria
2University Clinic of Pneumology, Paracelsus Medical University, Salzburg, Austria
Abstract
Since their discovery about fifteen years ago, neutrophil extracellular traps (NETs) have been recognized as an intrinsic part of vertebrate innate immunity and inflammatory response. Consisting of entangled strands of extracellular DNA decorated with histones, elastase, myeloperoxidase and other proteins, NETs entrap and kill pathogens, but are increasingly also found to contribute to acute and chronic inflammatory disease due to their toxicity to host cell and autoimmunity induction. Chronic obstructive pulmonary disease (COPD) turned out to be among the major disorders involving overshooting formation of NETs and associated adverse effect. In the present review, we summarize the progress in knowledge on the role of NETs in COPD pathology made since our first reports on this subject. We highlight recent substantial advances and discuss possible cause-and-effect relationships, connections with common comorbidities and interactions with drugs, also to illustrate the importance of NETs as a future diagnostic tool and target for new medication strategies.
Since their discovery about fifteen years ago, neutrophil extracellular traps (NETs) have been recognized as an intrinsic part of vertebrate innate immunity and inflammatory response. Consisting of entangled strands of extracellular DNA decorated with histones, elastase, myeloperoxidase and other proteins, NETs entrap and kill pathogens, but are increasingly also found to contribute to acute and chronic inflammatory disease due to their toxicity to host cell and autoimmunity induction. Chronic obstructive pulmonary disease (COPD) turned out to be among the major disorders involving overshooting formation of NETs and associated adverse effect. In the present review, we summarize the progress in knowledge on the role of NETs in COPD pathology made since our first reports on this subject. We highlight recent substantial advances and discuss possible cause-and-effect relationships, connections with common comorbidities and interactions with drugs, also to illustrate the importance of NETs as a future diagnostic tool and target for new medication strategies.
COPD is a progressive inflammatory airway disease, usually following long-term exposure to environmental insults. The main causal factor for developing COPD is inhaled tobacco smoke1. COPD affects around 10% of the adult population in industrialized countries2 and has substantial impact on the quality of life and life expectancy3. It is the third leading cause of death on the global scale4 and the sixth leading cause of death in countries with high socio-demographic index5. The disease varies in clinical presentation, often involving recurrent bacterial infection, massive neutrophil infiltration, and emphysematous alveolar wall destruction6. COPD is frequently still characterised into distinct ‘phenotypes’ based on varying criteria7–9 (caveats defined by Agusti10). In many cases, periods of stable condition alternate with episodes of worsening (exacerbations), leading to increasing small airway obstruction and lung function impairment. Lung function decline is also a key basis of disease assessment according to international guidelines11.
Extracellular traps (ETs) consist of entangled threads of DNA with dimensions down to 2 nm, associated with histones, elastase, myeloperoxidase (MPO) and other proteins that are antimicrobially effective, but also potentially cytotoxic12,13. ET formation (ETosis) by phagocytes is an intrinsic part of vertebrate innate pathogen defense and inflammatory response12. In humans, ETs are most frequently formed by neutrophils, then being abbreviated as NETs. Evidence on the existence of NETs is quite recent, first traces (although not explicitly designated) dating back to 199614, followed by a comprehensive description not until 200415. Since then, NET formation (NETosis) has turned out to be a versatile and multifaceted process with diverging signaling pathways and morphological execution12,16,17. NETosis is induced by a variety of host- or pathogen-derived molecular signals including chemokines such as inlerleukin-8 (IL-8), tumour necrosis factor alpha (TNFα), lipopolysaccharids, N-formylmethionyl-leucyl-phenylalanine (fMLP) and antineutrophil cytoplasmic antibodies (ANCAs), but also by calcium ionophores18,19 and pharmacological agents such as phorbol-12-myristate-13-acetate (PMA)12,15 and nicotine20,21. Some variants of NETosis including those assumed to be modifications of the autophagy pathway depend on reactive oxygen species (ROS) which may act on the process from both inside and outside the cell22–24. The main source of ROS involved in NETosis pathways are most probably subtypes of NADPH oxidase (Nox), but involvement of ROS from other sources (e.g. mitochondrial oxphos complexes, catalytic activity of myeloperoxidase, and nitric oxide synthase) is also proven25–29. ROS-independent NETosis is mediated by calcium ionophores19 and uric acid30. Transcriptome analyses have shown that DNA transcription at multiple chromosome loci during chromatin decondensation is a general feature of NETosis and occurs faster in the ROS-independent form than in the ROS/Nox-dependent form31. However, LPS- and PMA-induced NETs have been shown not to require protein translation for their formation, all necessary factors being already contained in the differentiated neutrophils emerging from bone marrow32.
Upon mitogenic stimulation and independent of ROS, NET-forming neutrophils were shown to employ the cell cycle kinases CDK4/6 for an incomplete activation of cell cycle reactions advancing until nuclear envelope breakdown33.
Before this background, nuclear chromatin is increasingly placed in a dual assignment, with a fully-fledged second function in immunity that combines direct anti-pathogen action with a prominent alerting role via activation of DNA receptors such as Toll-like receptor(TLR)-934.
The best described form of NETosis releases DNA from nuclear chromatin and leads to cell death12,35. Chromatin decondensation depending on histone citrullination by peptidyl arginine deiminase 4 (PAD4)36,37 is commonly regarded as a key feature of this type and used as an immunodiagnostic tool. Together with nuclear swelling, loss of intracellular organization, membrane rupture and extrusion of cell content, this constitutes a sequential morphological pattern also referred to as ‘NETotic cascade’12,38. Caveats resulting from recent re-evaluation of PAD-mediated citrullination24 require further consideration. Other mechanisms have been shown to leave NET-forming cells viable, and may also utilise mitochondrial DNA16,39.
Since their discovery15, NETs have been found to act in a fragile balance between beneficial and harmful. On the one hand, they aid the entrapment and removal of prokaryotic and eukaryotic pathogens40 (Fig. 1) and are also formed during viral infections41. On the other hand, NETs have been identified as toxic to host cells42, contributors to organ failure (e.g by interaction with platelets43), and potent inductors of autoimmunity44. Their formation in excess or in the wrong place, or their insufficient clearance, was found to be highly associated with severe acute illness and chronic inflammation45,46. This applies particularly to airway diseases such as allergic asthma47, cystic fibrosis (CF)48 and COPD.
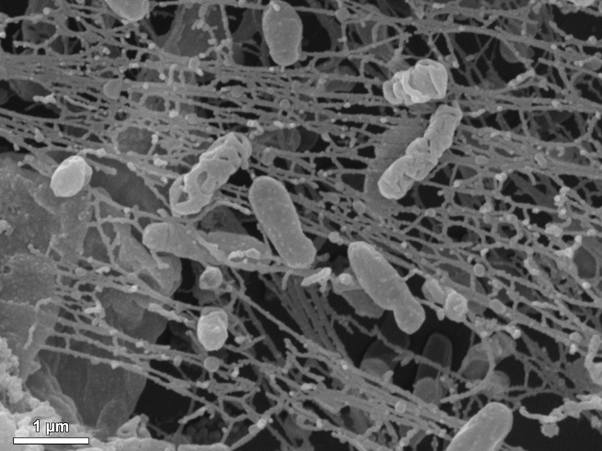
Figure 1: Scanning electron micrograph of in-vitro induced NETs entrapping Pseudomonas bacteria (Image: Astrid Obermayer, Salzburg).
Just like with CF, COPD had been a long-standing candidate for NETosis-mediated negative effects due to association with bacterial and viral infection49,50 and neutrophil infiltration6. Previous work from our lab using a combination of electron microscopy, fluorescence light microscopy and CLSM image-based morphometry has for the first time confirmed the presence of large amounts of NETs in the sputa of patients with exacerbated COPD. NET abundance was found to correlate with the degree of airflow limitation as measured by forced expiratory volume in one second (FEV1). We also found elevated NETosis in stable COPD and in smokers with still normal lung function13,51. These findings have since been substantially confirmed and expanded by the work of other groups: Extracellular DNA levels and content of NET associated protein in sputum has been shown to be significantly higher in COPD patients than in controls52,53, and spontaneous NET formation of neutrophils isolated from COPD sputum was found to be increased52. Interestingly, peripheral blood neutrophils of exacerbating COPD patients were found to diverge from those of stable COPD patients and controls in that they showed decreased in vitro NET formation in response to inflammatory stimuli, even though the plasma of the exacerbators contained elevated levels of extracellular DNA54. The culminating work to date is perhaps the comprehensive study of Dicker et al55. Applying a variety of methods to measure NET content in COPD sputa, these authors show a significant association between sputum NET concentrations and various parameters of disease severity. By presenting new assays for facilitated non-microscopy based quantification of NETs, they made an important step further toward making sputum NET content usable as a diagnostic tool applicable in routine laboratory analysis. By showing that sputum NET concentrations correlate with a decreased microbiome diversity, and that the presence of NETs reduces airway neutrophil phagocytosis, scientific progress was also achieved in testing the potential role of microbiota in this context. Other recent work using in vitro and ex vivo test systems has further corroborated the promotive role of cigarette smoke on ET formation by neutrophils and macrophages (METs), accompanied by the release of NE and matrix metalloproteinases (MMPs), and initiation of T-cell-mediated immune response56,57.
All this provides substantial support to the hypothesis that excess NET formation together with an unfavourable change in the phagocytosis/NETosis-balance58 impairs full clearance of bacterial infections in COPD airways, thus driving a self-perpetuating cycle of inflammation and NET formation, as already shown for cystic fibrosis59.
The increasing amount of data on the subject (evidence also comprehensively reviewed by Liu et al.60) encourages to further intensify research effort on the role of NETs in COPD, specifically to establish a more complete picture of the cause-and-effect relationships between the various aspects of the disease. Specific topics deserving to be further pursued concern molecular and biochemical interactions of intrinsic NETosis factors with the tissue environment (topics i – iv), and interrelations with individual circumstances of the disease, therapy and life cycle (topics v – viii).
(i) Histones. Core histones are known to account for 70% of all NET-associated proteins61, and nucleosome histone complexes are major structural constituents of fine NET threads13. Together with MPO, extracellular histones have been identified as main factors in NET-mediated cytotoxicity62. Signalling pathways involve Toll-like receptors, complement molecules, membrane-bound phospholipids, and proinflammatory chemokine release mediated by MyD88, NFκB, and inflammasomes63,64. Citrullinated histone H3 was found to evoke endothelial barrier dysfunction via opening of adherens junctions and promotion of stress fibre formation in the cytoskeleton65. The relevance of all this is still unproven for COPD, as is the extent to which histone co-aggregation with pentraxin 3 (PTX3), a further protein component of NETs, is able to protect COPD airway epithelia from histone-mediated cytotoxicity66.
(ii) Neutrophil elastase (NE). The serine protease NE (elastase 2) is another protein that is usually abundantly present in NETs. It has been attributed with a crucial role in emphysema development in animal model studies and human COPD already before NETs were first identified67. Over the years, a variety of animal models of emphysema induction by elastase instillation to the airways have been developed and tested, alone or in conjunction with other agents such as cigarette smoke, for suitability to mimic emphysema development at temporal, histological and molecular levels68–70. Regulatory pathways through which NE contributes to emphysema development are multifactorial and interdigitated, involving matrix metalloproteinases (MMPs), AMP-activated protein kinase (AMPK), α1,6-fucosyltransferase (Fut8), Wnt3a/b-catenin, and nuclear factor erythroid-2 related factor-2 (Nrf2), among others71,72. A relation to NADPH oxidase 2 (Nox)-dependent ROS production72,73 and ROS-mediated regulation of neutrophil interleukin?1 beta (IL?1β) secretion is obvious, differential coupling to pathways regulating autophagy and apoptosis seems probable74,75. However, it is unclear how all this contributes to the interdependency between NETosis and emphysema in COPD, – all the more so because the origin of extracellular NE may be diverse (see topic iii). An insufficiently explained side aspect in this context is also whether COPD emphysema and idiopathic pulmonary fibrosis (IPF) are in fact final conditions resulting from divergent derangement of a similar set of signalling pathways under similar noxious influence76.
(iii) Origin of neutrophil serine proteases (NSPs). Even when found associated with NETs, neutrophil proteases (in addition to NE also cathepsin G and proteinase 377) may derive from NETosis-independent exocytosis (degranulation) induced by various factors78,79, including macrolid antibiotics80. The contribution of NETosis-independent NSPs in COPD-related tissue damage may be substantial, not least due to secondary effects such as NSP-induced increased activation of proinflammatory cytokines (e.g. IL-1a, IL-36)81,82.
(iv) ETs formed by eosinophils (EETs) and macrophages (METs). Eosinophilic inflammation is a common phenotype in COPD83,84. Eosinophils have been shown to undergo at least two types of EET formation: cell death ETosis that cytolytically releases eosinophil granules85, and a specialised type of ETosis during which mitochondrial DNA is extruded in a catapult-like manner86. Recent research further strengthens a possible role of eosinophils in the pathophysiology of COPD phenotypes, notably already in the initial phase, and irrespective of whether patients quit smoking, with EETosis cell debris acting as a promoter of uncontrolled NETosis8. Recent work additionally suggests a relevant contribution of METs in COPD emphysema, especially under the influence of cigarette smoke56.
(v) Longitudinal relations. The information that NETosis intensity in COPD correlates with exacerbation derives mainly from cross sectional studies51,55, and provide no evidence on the course of NET levels through the sequence of exacerbations, their regressions, and intermittent stable phases in the individual patient. Accordingly, it is presently still impossible to discern whether increased NETosis is a result of, or a reason for exacerbations or whether NETs levels have an influence on the general progression of the disease.
(vi) Comorbidities. COPD is in many cases associated with comorbidities including lung cancer and other cancers, cardiovascular disease and diabetes. The crucial connecting factor appears to be systemic inflammation which is inherent to COPD and provides a promoting environment for various comorbidities87. In this context, ample evidence suggests that particularly the role of NETs and NET-components is worthy further examination. Deregulated inflammation with aberrant release of cytokines and ROS is known to generate a carcinogenic milieu in the lungs88, and NETs have been shown to be promotors of a tumorigenic microenvironment89. A similar association with NETosis has been established for cardiovascular disease including acute coronary syndrome46,90 and for diabetes91,92.
(vii) Drugs and stimulants. Influence on COPD NETosis by adjuvant medication and stimulants is as yet unexplored. Candidate substances among medical drugs include N-acetylcysteine (applied for routine mucolytic treatment) and phosphodiesterase (PDE4) inhibitors. In vitro data show that N-acetylcysteine is able to reduce the ability of human neutrophils to form NETs under low ROS levels93. Implications under the high and heterogeneous ROS levels in COPD airways94 are presently unexplored. PDE4 inhibitors are increasingly established in COPD medication to improve lung function and reduce the likelihood of exacerbations. Although there is as yet no direct evidence that PDE4 inhibitors affect NETosis, work on prostaglandin (PGE2) has shown that NETosis may be downregulated by cyclic adenosine monophosphate (cAMP). There is still no enquiry as to how PDE4 inhibitor-mediated elevated intracellular cAMP exerts influence on airway neutrophil NETosis. A further open issue in this context is NETosis promotion by nicotine20,21 in persistently smoking COPD subjects.
(viii) Influence of age. COPD-associated NETosis is linked to age-related phenomena in at least two ways: On the one hand, NETosis-driven chronic low-grade inflammation and high ROS levels accelerate tissue senescence via various molecular mechanisms also entailing depletion of precursor cells7,95,96. This designates NETosis as a major factor in lung ‘inflammaging’97,98, and supports the classification of COPD as a condition of accelerated/abnormal lung aging7,99. On the other hand, advancing age of both, the individual cells and the organism, modulates the neutrophils’ capacity to release NETs. This likely alters the balance of beneficial and detrimental effects of NETosis throughout the course of life in a complex and therapeutically relevant manner100.
In conclusion, the research in the wake of our first publications on the subject13,51 has to a large extent confirmed the hypothesis that NETosis levels in COPD correlate with disease severity, thus further highlighting the relevance of COPD-related NETosis as a promising target of diagnose and new medication strategies. Data available to date provide sound encouragement for several promising lines of research to be followed in the immediate future in order to improve the overall clinical outcome of the disease. The restricted scope of clinical trials on human patients highlights the need to improve and standardise preclinical in vitro and animal models for study of the NETosis-COPD relationship. This encourages effort to better adapt ex vivo-in vitro smoke models of NETosis induction57,101, and to standardise the diversity of animal COPD models (e.g.102,103) to facilitate representative validation of biomarkers and testing of therapy targets and new therapeutic agents. Refined in vitro and animal models may help to assess the effectiveness and side effects of NETosis inhibitors104–106. Prominently, knowledge about cooperative signalling in neutrophil recruitment and the as yet limited efficacy of cytokine blocking therapies in COPD107 may be expanded. Directions to be further followed are pointed by work comparing dual CXC-motiv-chemokine receptor 1/2 (CXCR1/2) inhibition vs. selective blocking of CXCR2108, or cooperative P-selectin glycoprotein ligand-1 (PSGL-1) and CXCR2 signaling in deep vein thrombosis109.
References
- Postma DS, Bush A, van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. The Lancet. 2015; 385: 899–909.
- Weiss G, Steinacher I, Lamprecht B, et al. Detection of Chronic Obstructive Pulmonary Disease in Primary Care in Salzburg, Austria: Findings from the Real World. Respiration, 2014; 87: 136–143.
- Calik-Kutukcu E, Savci S, Saglam M, et al. A comparison of muscle strength and endurance, exercise capacity, fatigue perception and quality of life in patients with chronic obstructive pulmonary disease and healthy subjects: a cross-sectional study. BMC Pulm Med. 2014; 14: 6.
- Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012; 380: 2095–2128.
- Wang H, Abajobir AA, Abate KH, et al. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017; 390: 1084–1150.
- Singh D, Edwards L, Tal-Singer R, et al. Sputum neutrophils as a biomarker in COPD: findings from the ECLIPSE study. Respir Res. 2010; 11: 77 – 89.
- Brandsma CA, Vries M de, Costa R, et al. Lung ageing and COPD: is there a role for ageing in abnormal tissue repair. Eur Respir Rev. 2017; 26: 170073.
- Uribe Echevarría L, Leimgruber C, García González J, et al. Evidence of eosinophil extracellular trap cell death in COPD: does it represent the trigger that switches on the disease. Int J Chron Obstruct Pulmon Dis. 2017; 12: 885–896.
- Miravitlles M, Calle M, Soler-Cataluña JJ. Clinical Phenotypes of COPD: Identification, Definition and Implications for Guidelines. Arch Bronconeumol Engl Ed. 2012; 48: 86–98.
- Agustí A. Phenotypes and Disease Characterization in Chronic Obstructive Pulmonary Disease. Toward the Extinction of Phenotypes. Ann Am Thorac Soc. 2013; 10: S125–S130.
- Vestbo J, Hurd SS, Agustí AG, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: GOLD Executive Summary. Am J Respir Crit Care Med. 2013; 187: 347–365.
- Remijsen Q, Kuijpers T, Wirawan E, et al. Dying for a cause: NETosis, mechanisms behind an antimicrobial cell death modality. Cell Death Differ. 2011; 18: 581–588.
- Obermayer A, Stoiber W, Krautgartner WD, et al. New aspects on the structure of neutrophil extracellular traps from chronic obstructive pulmonary disease and in vitro generation. PLoS ONE. 2014; 9: e97784.
- Takei H, Araki A, Watanabe H, et al. Rapid killing of human neutrophils by the potent activator phorbol 12-myristate 13-acetate (PMA) accompanied by changes different from typical apoptosis or necrosis. J Leukoc Biol. 1996; 59: 229–240.
- Brinkmann V, Reichard U, Goosmann C, et al. Neutrophil extracellular traps kill bacteria. Science. 2004; 303: 1532–1535.
- Pilsczek FH, Salina D, Poon KKH, et al. A novel mechanism of rapid nuclear neutrophil extracellular trap formation in response to Staphylococcus aureus. J Immunol. 2010; 185: 7413 – 7426.
- Parker H, Dragunow M, Hampton MB, et al. Requirements for NADPH oxidase and myeloperoxidase in neutrophil extracellular trap formation differ depending on the stimulus. J Leukoc Biol. 2012; 92: 841–849.
- Hoppenbrouwers T, Autar ASA, Sultan AR, et al. In vitro induction of NETosis: Comprehensive live imaging comparison and systematic review. PLOS ONE. 2017; 12: e0176472.
- Barrientos L, Marin-Esteban V, de Chaisemartin L, et al. An Improved Strategy to Recover Large Fragments of Functional Human Neutrophil Extracellular Traps. Front Immunol. 2013; 4. doi:10.3389/fimmu.2013.00166.
- Hosseinzadeh A, Thompson PR, Segal BH, et al. Nicotine induces neutrophil extracellular traps. J Leukoc Biol. 2016. doi:10.1189/jlb.3AB0815-379RR.
- Lee J, Luria A, Rhodes C, et al. Nicotine drives neutrophil extracellular traps formation and accelerates collagen-induced arthritis. Rheumatol Oxf Engl. 2017; 56: 644–653.
- Remijsen Q, Berghe TV, Wirawan E, et al. Neutrophil extracellular trap cell death requires both autophagy and superoxide generation. Cell Res. 2011; 21: 290–304.
- Douda DN, Khan MA, Grasemann H, et al. SK3 channel and mitochondrial ROS mediate NADPH oxidase-independent NETosis induced by calcium influx. Proc Natl Acad Sci. 2015; 112: 2817–2822.
- Konig MF, Andrade F. A Critical Reappraisal of Neutrophil Extracellular Traps and NETosis Mimics Based on Differential Requirements for Protein Citrullination. Front Immunol. 2016; 7. doi:10.3389/fimmu.2016.00461.
- Rochael NC, Guimarães-Costa AB, Nascimento MTC, et al. Classical ROS-dependent and early/rapid ROS-independent release of Neutrophil Extracellular Traps triggered by Leishmania parasites. Sci Rep. 2015; 5: 18302.
- Stoiber W, Obermayer A, Steinbacher P, et al. The Role of Reactive Oxygen Species (ROS) in the Formation of Extracellular Traps (ETs) in Humans. Biomolecules. 2015; 5: 702–723.
- Grayson PC, Kaplan MJ. At the Bench: Neutrophil extracellular traps (NETs) highlight novel aspects of innate immune system involvement in autoimmune diseases. J Leukoc Biol. 2016; 99: 253–264.
- Patel S, Kumar S, Jyoti A, et al. Nitric oxide donors release extracellular traps from human neutrophils by augmenting free radical generation. Nitric Oxide. 2010; 22: 226–234.
- Parker H, Winterbourn C. Reactive oxidants and myeloperoxidase and their involvement in neutrophil extracellular traps. Front Immunol. 2013; 3. doi:10.3389/fimmu.2012.00424.
- Arai Y, Nishinaka Y, Arai T, et al. Uric acid induces NADPH oxidase-independent neutrophil extracellular trap formation. Biochem Biophys Res Commun. 2013. doi:10.1016/j.bbrc.2013.12.007.
- Khan MA, Palaniyar N. Transcriptional firing helps to drive NETosis. Sci Rep. 2017; 7: 41749.
- Sollberger G, Amulic B, Zychlinsky A. Neutrophil Extracellular Trap Formation Is Independent of De Novo Gene Expression. PLOS ONE. 2016; 11: e0157454.
- Amulic B, Knackstedt SL, Abu Abed U, et al. Cell-Cycle Proteins Control Production of Neutrophil Extracellular Traps. Dev Cell. 2017; 43: 449-462.e5.
- Brinkmann V, Zychlinsky A. Neutrophil extracellular traps: Is immunity the second function of chromatin. J Cell Biol. 2012; 198: 773–783.
- Papayannopoulos V. Neutrophil extracellular traps in immunity and disease. Nat Rev Immunol. 2018; 18: 134–147.
- Neeli I, Khan SN, Radic M. Histone deimination as a response to inflammatory stimuli in neutrophils. JImmunol. 2008; 180: 1895–1902.
- Anzilotti C, Pratesi F, Tommasi C, et al. Peptidylarginine deiminase 4 and citrullination in health and disease. Autoimmun Rev. 2010; 9: 158–160.
- Fuchs TA, Abed U, Goosmann C, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol. 2007; 176: 231–241.
- Yousefi S, Mihalache C, Kozlowski E, et al. Viable neutrophils release mitochondrial DNA to form neutrophil extracellular traps. Cell Death Differ. 2009; 16: 1438 – 1444.
- Guimarães-Costa AB, Nascimento MTC, Wardini AB, et al. ETosis: A Microbicidal Mechanism beyond Cell Death. J Parasitol Res. 2012; 2012: 929743.
- Jenne CN, Wong CHY, Zemp FJ, et al. Neutrophils recruited to sites of infection protect from virus challenge by releasing neutrophil extracellular traps. Cell Host Microbe. 2013; 13: 169–180.
- Narasaraju T, Yang E, Samy RP, et al. Excessive Neutrophils and Neutrophil Extracellular Traps Contribute to Acute Lung Injury of Influenza Pneumonitis. Am J Pathol. 2011; 179: 199–210.
- McDonald B, Davis RP, Kim SJ, et al. Platelets and neutrophil extracellular traps collaborate to promote intravascular coagulation during sepsis in mice. Blood. 2017; 129: 1357–1367.
- Khandpur R, Carmona-Rivera C, Vivekanandan-Giri A, et al. NETs are a source of citrullinated autoantigens and stimulate inflammatory responses in rheumatoid arthritis. Sci Transl Med. 2013; 5: 178ra40.
- Kaplan MJ, Radic M. Neutrophil extracellular traps: Double-edged swords of innate immunity. J Immunol. 2012; 189: 2689–2695.
- Mangold A, Alias S, Scherz T, et al. Coronary neutrophil extracellular trap burden and deoxyribonuclease activity in ST-elevation acute coronary syndrome are predictors of ST-segment resolution and infarct size. Circ Res. 2015; 116: 1182–1192.
- Dworski R, Simon HU, Hoskins A, et al. Eosinophil and neutrophil extracellular DNA traps in human allergic asthmatic airways. J Allergy Clin Immunol. 2011; 127: 1260–1266.
- Marcos V, Zhou-Suckow Z, Önder Yildirim A, et al. Free DNA in Cystic Fibrosis Airway Fluids Correlates with Airflow Obstruction. Mediators Inflamm. 2015; 2015: 408935.
- George SN, Garcha DS, Mackay AJ, et al. Human rhinovirus infection during naturally occurring COPD exacerbations. Eur Respir J. 2014; 44: 87–96.
- Huang YJ, Sethi S, Murphy T, et al. Airway Microbiome Dynamics in Exacerbations of Chronic Obstructive Pulmonary Disease. J Clin Microbiol. 2014; 52: 2813–2823.
- Grabcanovic-Musija F, Obermayer A, Stoiber W, et al. Neutrophil extracellular trap (NET) formation characterises stable and exacerbated COPD and correlates with airflow limitation. Respir Res. 2015; 16: 59.
- Pedersen F, Marwitz S, Holz O, et al. Neutrophil extracellular trap formation and extracellular DNA in sputum of stable COPD patients. Respir Med. 2015. doi:10.1016/j.rmed.2015.08.008.
- Wright TK, Gibson PG, Simpson JL, et al. Neutrophil extracellular traps are associated with inflammation in chronic airway disease. Respirology. 2016. doi:10.1111/resp.12730.
- Pullan J, Hannah Greenwood, Georgia M Walton, et al. Stockley, Elizabeth Sapey. Neutrophil extracellular traps (NETs) in COPD: A potential novel mechanism for host damage in acute exacerbations. Eur Respir J. 2015; 46: PA5055.
- Dicker AJ, Crichton ML, Pumphrey EG, et al. Neutrophil extracellular traps are associated with disease severity and microbiota diversity in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018; 141: 117–127.
- King PT, Sharma R, O’Sullivan KM, et al. Deoxyribonuclease 1 reduces pathogenic effects of cigarette smoke exposure in the lung. Sci Rep. 2017; 7: 12128.
- Qiu SL, Zhang H, Tang Q, et al. Neutrophil extracellular traps induced by cigarette smoke activate plasmacytoid dendritic cells. Thorax. 2017; 72: 1084–1093.
- Branzk N, Lubojemska A, Hardison SE, et al. Neutrophils sense microbe size and selectively release neutrophil extracellular traps in response to large pathogens. Nat Immunol. 2014; 15: 1017–1025.
- Yoo D, Winn M, Pang L, et al. Release of Cystic Fibrosis Airway Inflammatory Markers from Pseudomonas aeruginosa–Stimulated Human Neutrophils Involves NADPH Oxidase-Dependent Extracellular DNA Trap Formation. J Immunol. 2014; 192: 4728–4738.
- Liu T, Wang FP, Wang G, et al. Role of Neutrophil Extracellular Traps in Asthma and Chronic Obstructive Pulmonary Disease. Chin Med J (Engl). 2017; 130: 730–736.
- Urban CF, Ermert D, Schmid M, et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 2009; 5: e1000639.
- Saffarzadeh M, Juenemann C, Queisser MA, et al. Neutrophil extracellular traps directly induce epithelial and endothelial cell death: A predominant role of histones. PLoS ONE. 2012; 7: e32366.
- Hoeksema M, van Eijk M, Haagsman HP, et al. Histones as mediators of host defense, inflammation and thrombosis. Future Microbiol. 2016; 11: 441–453.
- Silk E, Zhao H, Weng H, et al. The role of extracellular histone in organ injury. Cell Death Dis. 2017; 8: e2812.
- Meegan JE, Yang X, Beard RS, et al. Citrullinated histone 3 causes endothelial barrier dysfunction. Biochem Biophys Res Commun. 2018; 503: 1498–1502.
- Daigo K, Takamatsu Y, Hamakubo T. The Protective Effect against Extracellular Histones Afforded by Long-Pentraxin PTX3 as a Regulator of NETs. Front Immunol. 2016; 7. doi:10.3389/fimmu.2016.00344.
- Shapiro SD, Goldstein NM, Houghton AM, et al. Neutrophil Elastase Contributes to Cigarette Smoke-Induced Emphysema in Mice. Am J Pathol. 2003; 163: 2329–2335.
- Inoue K, Koike E, Yanagisawa R, et al. Extensive Analysis of Elastase-Induced Pulmonary Emphysema in Rats: ALP in the Lung, a New Biomarker for Disease Progression. J Clin Biochem Nutr. 2010; 46: 168–176.
- Oliveira MV, Abreu SC, Padilha GA, et al. Characterization of a Mouse Model of Emphysema Induced by Multiple Instillations of Low-Dose Elastase. Front Physiol. 2016; 7. doi:10.3389/fphys.2016.00457.
- Suki B, Bartolák-Suki E, Rocco PRM. Elastase-Induced Lung Emphysema Models in Mice. Methods Mol Biol Clifton NJ. 2017; 1639: 67–75.
- Kamio K, Yoshida T, Gao C, et al. α1,6-Fucosyltransferase (Fut8) is implicated in vulnerability to elastase-induced emphysema in mice and a possible non-invasive predictive marker for disease progression and exacerbations in chronic obstructive pulmonary disease (COPD). Biochem Biophys Res Commun. 2012; 424: 112–117.
- Cui W, Zhang Z, Zhang P, et al. Nrf2 attenuates inflammatory response in COPD/emphysema: Crosstalk with Wnt3a/β-catenin and AMPK pathways. J Cell Mol Med. 2018; 22: 3514–3525.
- Khan MA, Philip LM, Cheung G, et al. Regulating NETosis: Increasing pH Promotes NADPH Oxidase-Dependent NETosis. Front Med. 2018; 5. doi:10.3389/fmed.2018.00019.
- Gabelloni ML, Sabbione F, Jancic C, et al. NADPH oxidase derived reactive oxygen species are involved in human neutrophil IL-1β secretion but not in inflammasome activation. Eur J Immunol. 2013; 43: 3324–3335.
- Iula L, Keitelman IA, Sabbione F, et al. Autophagy Mediates Interleukin-1β Secretion in Human Neutrophils. Front Immunol. 2018; 9. doi:10.3389/fimmu.2018.00269.
- Chilosi M, Poletti V, Rossi A. The pathogenesis of COPD and IPF: Distinct horns of the same devil. Respir Res. 2012; 13: 3.
- Pham CTN. Neutrophil serine proteases: specific regulators of inflammation. Nat Rev Immunol. 2006; 6: 541–550.
- Kessenbrock K, Dau T, Jenne DE. Tailor-made inflammation: how neutrophil serine proteases modulate the inflammatory response. J Mol Med. 2011; 89: 23–28.
- Kettritz R. Neutral serine proteases of neutrophils. Immunol Rev. 2016; 273: 232–248.
- Abdelghaffar H, Vazifeh D, Labro MT. Comparison of various macrolides on stimulation of human neutrophil degranulation in vitro. J Antimicrob Chemother. 1996; 38: 81–93.
- Henry CM, Sullivan GP, Clancy DM, et al. Neutrophil-Derived Proteases Escalate Inflammation through Activation of IL-36 Family Cytokines. Cell Rep. 2016; 14: 708–722.
- Clancy DM, Henry CM, Sullivan GP, et al. Neutrophil extracellular traps can serve as platforms for processing and activation of IL-1 family cytokines. FEBS J. 2017; 284: 1712–1725.
- Kim VL, Coombs NA, Staples KJ, et al. Impact and associations of eosinophilic inflammation in COPD: analysis of the AERIS cohort. Eur Respir J. 2017; 50: 1700853.
- Ortega H, Llanos JP, Lafeuille MH, et al. Burden of disease associated with a COPD eosinophilic phenotype. Int J Chron Obstruct Pulmon Dis. 2018; 13: 2425–2433.
- Ueki S, Melo RCN, Ghiran I, et al. Eosinophil extracellular DNA trap cell death mediates lytic release of free secretion competent eosinophil granules. Blood. 2013; 121: 2074–2083.
- Yousefi S, Gold JA, Andina N, et al. Catapult-like release of mitochondrial DNA by eosinophils contributes to antibacterial defense. Nat Med. 2008; 14: 949–953.
- Hillas G, Perlikos F, Tsiligianni I, et al. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015; 10: 95–109.
- Vermaelen K, Brusselle G. Exposing a deadly alliance: Novel insights into the biological links between COPD and lung cancer. Pulm Pharmacol Ther. 2013; 26: 544–554.
- Jorch SK, Kubes P. An emerging role for neutrophil extracellular traps in noninfectious disease. Nat Med. 2017; 23: 279–287.
- Delabranche X, Stiel L, Severac F, et al. Evidence of Netosis in Septic Shock-induced Disseminated Intravascular Coagulation. Shock. 2017; 47: 313–317.
- Wang Y, Xiao Y, Zhong L, et al. Increased Neutrophil Elastase and Proteinase 3 and Augmented NETosis Are Closely Associated With β-Cell Autoimmunity in Patients With Type 1 Diabetes. Diabetes. 2014; 63: 4239–4248.
- Wong SL, Demers M, Martinod K, et al. Diabetes primes neutrophils to undergo NETosis, which impairs wound healing. Nat Med. 2015; 21: 815–819.
- Zawrotniak M, Kozik A, Rapala-Kozik M. Selected mucolytic, anti-inflammatory and cardiovascular drugs change the ability of neutrophils to form extracellular traps (NETs). Acta Biochim Pol. 2015; 62: 465–473.
- Boukhenouna S, Wilson MA, Bahmed K, et al. Reactive Oxygen Species in Chronic Obstructive Pulmonary Disease. Oxid Med Cell Longev. 2018; 2018: 5730395.
- Chilosi M, Carloni A, Rossi A, et al. Premature lung aging and cellular senescence in the pathogenesis of idiopathic pulmonary fibrosis and COPD/emphysema. Transl Res. 2013; 162: 156–173.
- Ghosh M, Miller YE, Nakachi I, et al. Exhaustion of Airway Basal Progenitor Cells in Early and Established Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2018; 197: 885–896.
- Sundar IK, Yao H, Rahman I. Oxidative Stress and Chromatin Remodeling in Chronic Obstructive Pulmonary Disease and Smoking-Related Diseases. Antioxid Redox Signal. 2013; 18: 1956–1971.
- Kovacs EJ, Boe DM, Boule LA, et al. Inflammaging and the Lung. Clin Geriatr Med. 2017; 33: 459–471.
- MacNee W. Is Chronic Obstructive Pulmonary Disease an Accelerated Aging Disease? Ann Am Thorac Soc. 2016; 13: S429–S437.
- Ortmann W, Kolaczkowska E. Age is the work of art? Impact of neutrophil and organism age on neutrophil extracellular trap formation. Cell Tissue Res. 2018; 371: 473–488.
- Bokaba RP, Anderson R, Theron AJ, et al. Cigarette smoke condensate attenuates phorbol ester-mediated neutrophil extracellular trap formation. Afr Health Sci. 2017; 17: 896–904.
- Ghorani V, Boskabady MH, Khazdair MR, et al. Experimental animal models for COPD: a methodological review. Tob Induc Dis. 2017; 15: 25.
- Jones B, Donovan C, Liu G, et al. Animal models of COPD: What do they tell us. Respirology 2017; 22: 21–32.
- Ohbayashi H. Neutrophil elastase inhibitors as treatment for COPD. Expert Opin Investig Drugs. 2002; 11: 965–980.
- Cools-Lartigue J, Spicer J, McDonald B, et al. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J Clin Invest. 2013; 123: 3446–3458.
- Sabbione F, Keitelman IA, Iula L, et al. Neutrophil Extracellular Traps Stimulate Proinflammatory Responses in Human Airway Epithelial Cells. J Innate Immun. 2017; 9: 387–402.
- Caramori G, Adcock IM, Di Stefano A, et al. Cytokine inhibition in the treatment of COPD. Int J Chron Obstruct Pulmon Dis. 2014; 9: 397–412.
- Planagumà A, Domènech T, Pont M, et al. Combined anti CXC receptors 1 and 2 therapy is a promising anti-inflammatory treatment for respiratory diseases by reducing neutrophil migration and activation. Pulm Pharmacol Ther. 2015; 34: 37–45.
- Yago T, Liu Z, Ahamed J, et al. Cooperative PSGL-1 and CXCR2 signaling in neutrophils promotes deep vein thrombosis in mice. Blood. 2018; 132: 1426–1437.
