Children Protection Against COVID-19 at the Pandemic Outbreak
Dana Khdr Sabir1*, Nabaz R. Khwarahm2, Shakhawan M. Ali3, Hayman J Abdoul4, Kochar I. Mahmood5, Rimantas Kodzius6,7*
1Department of Medical Laboratory Sciences, Charmo University, 46023 Chamchamal, Kurdistan Region, Iraq
2Department of Biology, College of Education, University of Sulaimani, Sulaimani, Kurdistan Region, Iraq
3Department of Oral and Maxillofacial Surgery, School of Medicine, Faculty of Dentistry, University of Sulaimani,Sulaimani, Kurdistan Region, Iraq
4Department of Pharmaceutical Chemistry, Charmo University, 46023 Chamchamal, Kurdistan Region, Iraq
5Charmo Centre for Research, Training and Consultancy, Charmo University, 46023 Chamchamal, Kurdistan Region, Iraq
6Kaunas Technology University (KTU), 37164 Panevezys, Lithuania
7Ludwig Maximilian University of Munich (LMU), 80539 Munich, Germany
Abstract
Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) is a novel strain of coronavirus that is recently identified as an etiological agent for the current pandemic respiratory illness called coronavirus disease 2019 (COVID-19). The disease might have a zoonotic origin and has infected > 19 million people around the globe with > 700,000 deaths. The published data indicate that children are generally less susceptible to contracting COVID-19. Here, we are providing a review on current hypotheses that have tried to explain the low mortality and morbidity rate among children. We believe that understanding the immunological base of children’s protection can prevent further spread of the disease.
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease of the human respiratory system caused by a novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The disease was first reported in Wuhan/ China in December 2019 and now it has spread globally, resulting in the on-going COVID-19 pandemic1. The disease can spread human-to-human mainly through contaminated aerosol droplets of coughing or sneezing2. As of 4 of June, more than 6.4 million laboratory-confirmed infections and 380, 000 deaths by COVID-19 recorded3.
Released data from the affected countries are showing that children under 10 years old are generally less susceptible to the virus infection and usually are asymptomatic or suffer from milder symptoms with lower fatality rates compared to the adults or elderly people4-6. In Italy, for instance, 2 children died out of 20,531 COVID-19 deaths by April 17, 2020 (Figure 1)7. The death of one child was also reported in Spain among 382 infected children out of 122.818 confirmed cases in the country8. In South Korea, no mortality is recorded among 1.09% infected children out of 10,653 confirmed COVID-19 patients9 (Figure 1). The morbidity and mortality of children with COVID-19 were 0.9% and 0% respectively among 72,314 infected people in China10. In France and the USA, the children's mortality numbers to the total deaths recorded are 0/6507 death11 and 3/13,13012, respectively. Cascella et al. (2020) were also pointed out that children are less affected by the disease, but they can transmit the disease to other people13. Infants ( less than 1-year-old), however, are appeared to be susceptible to the disease14. Although, COVID-19 was initially thought that cannot be transmitted from the mothers to their newborns15-17, a report by Vivanti A. et al (2020)18 demonstrated transplacental transmission of SARS-CoV-2 from a pregnant COVID-19 infected woman to her newborn18. Yet, the adults and elderly people are vulnerable to the disease, particularly those who have some underlying health conditions19.
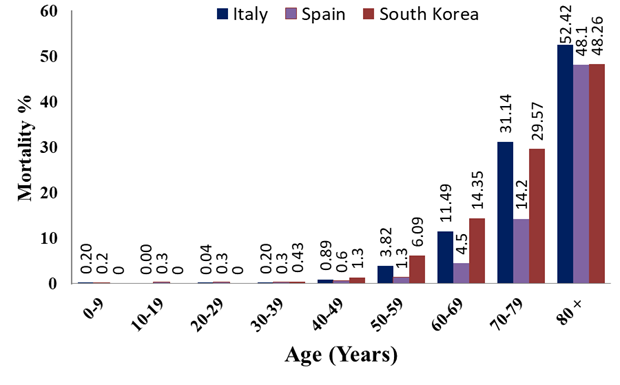
Figure 1: Age distribution of COVID-19 mortality rate in Italy, Spain, and South Korea.
Sign and symptoms of the Disease
COVID-19 is an infectious disease of the human respiratory system illness20. The general signs and symptoms of the disease are flu-like symptoms such as fever, dry cough, fatigue, headache, sore throat, shortness of breath and myalgia and in rare cases nausea, vomiting and diarrhoea have occurred2,21,22. Dong Y et al. (2020)14 demonstrated that the children with COVID-19 generally showed less severe clinical manifestations in comparison to those of adults’ patients14. In a systematic review of COVID-19 in children, Ludvigsson, J. F. (2020), demonstrated that children have so far accounted for only 1%-5% of diagnosed COVID-19 cases; they often have milder disease than adults and deaths by the disease is extremely rare22. Accordingly, the prevalence of severe and critical disease was 10.6% in children aged below 1 year, and 7.3% in 1-5 years children, while for those aged between 6-10 and 11-15 years were about 4.1%, and 3.0% for children with 16-17 years old22.
In a study that performed on 41 laboratory-confirmed COVID-19 patients in Wuhan hospital in early January 2020, no children or adolescents were recorded and most of the infected patients were men (73%)20. All the identified cases had pneumonia with abnormal findings on chest CT, in which fever was considered as a common symptom at onset of illness (98%) and this followed by cough which was found in 31 out of 41 patients (76%), further, feeling of fatigue and myalgia was appeared in 44% of patients, whereas the production of sputum not much common as the other symptoms (28%) and only three cases had headache20. Recent reports suggest a new clinical syndrome, with significant inflammation and similarities to Kawasaki disease, related with SARS-CoV-2 infection among children. Wide ranges of symptoms have been reported for this syndrome such as cardiac disease, mild or absent respiratory symptoms, and variable incidence of rash, red eyes, and oral mucous membrane changes23.
Etiology of the disease
COVID-19 is caused by SARS-Cov-2; a genus of a large Coronaviridae family, which are positive single-stranded RNA viruses24. SARS-CoV-2, with the other two previously identified human pathogens: SARS-CoV and MERS-CoV, belong to the β-genus of the family25. Genome size of the Coronaviruses are ranged between 26 to 32 Kbp which encoded for at least 6 open reading frames (ORFs)24. Figure 2 shows the schematic representation of the first genome sequence of the SARS-CoV-2 (Accession number: MN908947) which was isolated in Wuhan China25. At least 12 ORFs were predicted in the 29,903 nucleotides genome size of the virus including Spike (S) glycoprotein. This protein plays a critical role in the pathogenicity of the virus by medicating virus-cell fusion through binding to the same human cell receptor called the angiotensin-converting enzyme 2 (ACE2)25. Thus, Spike (S) glycoprotein protein is considered as an important therapeutic and diagnostic target of the disease. The structure of the S protein was determined using cryo-electron microscopy (PDB: 6VSB)26. It has shown that SARS-CoV S protein shares high sequence similarity to SARS-COV-2, however, the latter protein has 10 times more affinity towards human’s ACE 2 compared to SARS-CoV26. Such high affinity can explain why COVID-19 can spread easier from a human to human compared to either MERS or SARS-CoV.
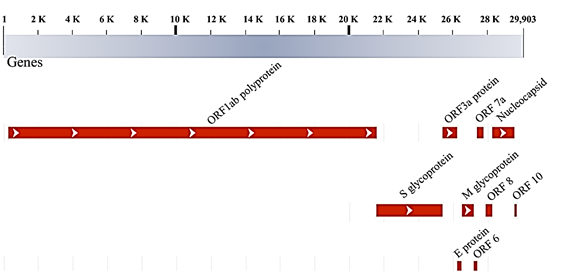
Figure 2: Schematic representation of SARS-CoV-2 genome and the proteins encoded (Accession number: MN908947.3)25.
Discussion
Mortality and morbidity of COVID-19’s cases are increasing on a daily bases, yet there is not an effective vaccine available against the virus, despite trials of 150 vaccine types worldwide27, except for proposing some therapeutic clues for patients with underlined conditions (e.g., diabetes mellitus)28. The best way to reduce losing lives is by protecting vulnerable groups.
Children appear to be less susceptible to COVID-19’s infection. It was proposed that T-cells play an important role in protecting children against the COVID-1929. This is because children have a large number of naive T-cells, which can be programmed by new pathogens, this in turn provides advantageous protection compared to the elderly people30. In addition, pre-existing T- cells immunity acquired from previous coronaviruses or common cold infections could also protect children from COVID-19. SARS-CoV-2 specific T- cells have been reported in both SARS-recovered and uninfected people31. Moreover, the presence of the viruses that commonly found in the mucosa of lungs and airways of children may protect the children and limit the growth of SARS-CoV2 through virus-to-virus competition32. The latter hypothesis supported by the fact that there is a direct link between the viral load and clinical symptoms of the patients: the higher the viral copies, more severe the disease is33. We should mention that this argument is only valid for children with no underlying medical conditions, for example, asthma and other respiratory conditions.
Moreover, ACE2; a receptor that is required for SARS-Cov2 binding and infection34, may have a lower expression level or binding capacities in children compared to the adults35. Indeed, a recent study conducted among a group of 305 patient aged 4 to 60 years old has shown age-dependent ACE2 gene expression in nasal epithelium, with the lowest expression of the gene in the children younger than 10 years old36. It is already known that the higher expression level of ACE2 increases the susceptibility of the people to the entry of the viral host cell and propagation37.
The role of early childhood vaccinations, particularly Bacille Calmette-Guérin (BCG) and measles, mumps, and rubella (MMR) vaccines, has received a great attention worldwide38,39. It is known that Children are generally vaccinated against numbers of bacterial and viral infections such as tuberculosis, diphtheria, tetanus, pertussis, measles, rubella, hepatitis A, hepatitis B40. It is possible that the antibodies produced in the case of one or more of the above vaccination may cross-reacts with the antigenic epitopes of spike (S) protein. Interestingly, a short sequence (30 amino acids) homology has been detected between SARS-CoV-2 Spike (S) glycoprotein and measles virus fusion (F1) glycoprotein as well as rubella virus envelope (E1) glycoprotein in the possible antigenic epitopes region39. In addition, stronger children protection against COVID-19 in comparison to adults or elderly could be due to the fact that the antibody titers of the above vaccine prevented disease decrease over the time41. Previously, a cross-protection immune response against the lethal 1918 Spanish influenza A virus was also reported through the 2009 H1N1 influenza virus vaccine42. Human sharing immunity was also reported between Zika and Dengue fever viruses23. Lastly, some argue that children protection against COVID-19 does not have an immunity base; it is rather related to human behavior and life style in which children are generally well-cared at home and have fewer chances to get exposed to the infected people14. Lee, Hu et al. (2020) also supported this suggestion that children are less prone to international travelling and outdoor activities. However, this suggestion may greatly change if different age group of children were exposed to transmission factors of the virus (e.g. outdoor activities and exposure)43.
Recommendation
Taking into account the current evidences that children are less prone to COVID-19 and hence are in the low-risk category zone. Yet, keeping schools closed and restricting children from normal social activities may lead to develop metal health issues44. Therefore, children should be trained to acquire behaviors of protecting themselves and their surroundings from contracting and then spreading the virus. This can be done by educating children about the germs in general and viruses in particular, as necessary and basic preventive actions.
The preventive actions that should be taught to children as recommended by Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO)45,46, could include, but not limited to the following:
1- Washing hands frequently to minimize spreading the virus (i.e., soap and water for 20 seconds before eating). Children can be taught to use hand hygiene gel but, but this needs to be done under adult supervision to avoid toxicity.
2- Minimize touching random surfaces
3- Wearing masks and gloves by children as well as adults in the crowd places
4- Minimize interacting with adults in general, particularly those who suffer from flu-like symptoms (e.g. sneezing, coughing, and fever)
5- Avoiding close contact with infected family members during lockdown and home-quarantine.
6- Seek information from local health authorities about the Coronavirus epidemic.
Conclusion
Overall, released data are strongly suggesting two views: (i) that children are less susceptible to COVID-19 compared to adult or elderly people. This is either through innate immunity or acquired immunity or perhaps a lower expression of the ACE2 receptor cells in children. Therefore, understanding the cellular mechanism of the children's protection could help to prevent and/or reduce the further spreading of the virus (ii) Children with COVID-19 may show little or no symptoms. This should be taken into consideration with caution as they may play as a spreading factor. The suggested immunity and lifestyle factors that make children less prone to the COVID-19 remain as open questions (i.e. hypotheses) and yet to be investigated further.
References
- Wang, C., P.W. Horby, F.G. Hayden, and G.F. Gao, A novel coronavirus outbreak of global health concern. The Lancet, 2020. 395(10223): p. 470-473.
- Mahmud, P.K., S.M. Ali, and D.K. Sabir, Impacts of novel pandemic coronavirus (COVID-19) outbreak on dental practice: A review of the. 2020.
- World Health Organization (Report: 136), Coronavirus disease 2019 (COVID-19): situation report- 136 (Accessed on 4 June, 2020). 2020.
- Brodin, P., Why is COVID-19 so mild in children? Acta Paediatr, 2020. 109(6): p. 1082-1083.
- Xu, Y., X. Li, B. Zhu, H. Liang, C. Fang, Y. Gong, Q. Guo, X. Sun, D. Zhao, and J. Shen, Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nature medicine, 2020: p. 1-4.
- Alsayed, R., M. Kadhom, E. Yousif, and D.K. Sabir, An Epidemiological Characteristic of the COVID-19 Among Children. Letters in Applied NanoBioScience, 2020. 9(3): p. 1156 - 1164.
- Italian National Institute of Health (ISS), del Dipartimento Malattie Infettive e Servizio di Informatica. Sorveglianza integrata covid-19 in italia. 2020. 2020.
- Ministry of Health Social Services and Equality, Actualización nº 75. Enfermedad por el coronavirus (COVID-19)Actualización nº 67. Enfermedad por el coronavirus (COVID-19), page 2. 2020.
- Korean Centers for Disease Control & Prevention (KCDC), Updates on COVID-19 in Republic of Korea. 2020: Korean Centers for Disease Control & Prevention (KCDC). URL: www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 )Ù(Access on April 18, 2020).
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi, 2020. 41(2): p. 145-151.
- Public Health of France, COVID-19: Point épidémiologique - Situation au 15 mars 2020 à minuit (https://www.santepubliquefrance.fr/) (Accessed on March 15, 2020). 2020
- Centers for Disease Control and Prevention (CDC), Provisional Death Counts for Coronavirus Disease (COVID-19) (https://www.cdc.gov/nchs/nvss/vsrr/COVID19/index.htm, Accessed on April 19, 2020). 2020.
- Cascella, M., M. Rajnik, A. Cuomo, S.C. Dulebohn, and R. Di Napoli, Features, Evaluation and Treatment Coronavirus (COVID-19), in StatPearls [Internet]. 2020, StatPearls Publishing.
- Dong, Y., X. Mo, Y. Hu, X. Qi, F. Jiang, Z. Jiang, and S. Tong, Epidemiology of COVID-19 among children in China. Pediatrics, 2020.
- Schwartz, D.A., An Analysis of 38 Pregnant Women With COVID-19, Their Newborn Infants, and Maternal-Fetal Transmission of SARS-CoV-2: Maternal Coronavirus Infections and Pregnancy Outcomes. Archives of Pathology & Laboratory Medicine, 2020. 144(7): p. 799-805.
- Zhu, H., L. Wang, C. Fang, S. Peng, L. Zhang, G. Chang, S. Xia, and W. Zhou, Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Translational Pediatrics, 2020. 9(1): p. 51-60.
- Chen, H., J. Guo, C. Wang, F. Luo, X. Yu, W. Zhang, J. Li, D. Zhao, D. Xu, Q. Gong, J. Liao, H. Yang, W. Hou, and Y. Zhang, Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet, 2020. 395(10226): p. 809-815.
- Vivanti, A., C. Vauloup-Fellous, S. Prevot, V. Zupan, C. Suffee, J. Do Cao, A. Benachi, and D. De Luca, Transplacental transmission of SARS-CoV-2 infection. 2020.
- Remuzzi, A. and G. Remuzzi, COVID-19 and Italy: what next? The Lancet, 2020.
- Huang, C., Y. Wang, X. Li, L. Ren, J. Zhao, Y. Hu, L. Zhang, G. Fan, J. Xu, and X. Gu, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 2020. 395(10223): p. 497-506.
- Zimmermann, P. and N. Curtis, Coronavirus Infections in Children Including COVID-19: An Overview of the Epidemiology, Clinical Features, Diagnosis, Treatment and Prevention Options in Children. The Pediatric Infectious Disease Journal, 2020. 39(5): p. 355-368.
- Ludvigsson, J.F., Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica, 2020. 109(6): p. 1088-1095.
- Hennon, T.R., M.D. Penque, R. Abdul-Aziz, O.S. Alibrahim, M.B. McGreevy, A.J. Prout, B.A. Schaefer, S.J. Ambrusko, J.V. Pastore, S.J. Turkovich, O.G. Gomez-Duarte, and M.D. Hicar, COVID-19 associated Multisystem Inflammatory Syndrome in Children (MIS-C) guidelines; a Western New York approach. Progress in Pediatric Cardiology, 2020: p. 101232.
- Perlman, S. and J. Netland, Coronaviruses post-SARS: update on replication and pathogenesis. Nature Reviews Microbiology, 2009. 7(6): p. 439-450.
- Wu, F., S. Zhao, B. Yu, Y.-M. Chen, W. Wang, Z.-G. Song, Y. Hu, Z.-W. Tao, J.-H. Tian, and Y.-Y. Pei, A new coronavirus associated with human respiratory disease in China. Nature, 2020. 579(7798): p. 265-269.
- Wrapp, D., N. Wang, K.S. Corbett, J.A. Goldsmith, C.-L. Hsieh, O. Abiona, B.S. Graham, and J.S. McLellan, Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science, 2020. 367(6483): p. 1260-1263.
- Kandimalla, R., A. John, C. Abburi, J. Vallamkondu, and P.H. Reddy, Current Status of Multiple Drug Molecules, and Vaccines: An Update in SARS-CoV-2 Therapeutics. Molecular neurobiology, 2020: p. 1-11.
- Vallamkondu, J., A. John, W.Y. Wani, S.P. Ramadevi, K.K. Jella, P.H. Reddy, and R. Kandimalla, SARS-CoV-2 pathophysiology and assessment of coronaviruses in CNS diseases with a focus on therapeutic targets. Biochimica et biophysica acta. Molecular basis of disease, 2020. 1866(10): p. 165889-165889.
- Sabir, D.K., K.R. Sidiq, and S.M. Ali, Current Speculations on the Low Incidence Rate of the COVID-19 among Children. International Journal of School Health, 2020. 7(2): p. 37-38.
- Ahmadpoor, P. and L. Rostaing, Why the immune system fails to mount an adaptive immune response to a Covidâ19 infection. Transplant International, 2020.
- Le Bert, N., A.T. Tan, K. Kunasegaran, C.Y. Tham, M. Hafezi, A. Chia, M.H.Y. Chng, M. Lin, N. Tan, and M. Linster, SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature, 2020: p. 1-10.
- Nickbakhsh, S., C. Mair, L. Matthews, R. Reeve, P.C. Johnson, F. Thorburn, B. von Wissmann, A. Reynolds, J. McMenamin, and R.N. Gunson, Virus–virus interactions impact the population dynamics of influenza and the common cold. Proceedings of the National Academy of Sciences, 2019. 116(52): p. 27142-27150.
- Liu, Y., L.-M. Yan, L. Wan, T.-X. Xiang, A. Le, J.-M. Liu, M. Peiris, L.L. Poon, and W. Zhang, Viral dynamics in mild and severe cases of COVID-19. The Lancet Infectious Diseases, 2020.
- Zhou, P., X.-L. Yang, X.-G. Wang, B. Hu, L. Zhang, W. Zhang, H.-R. Si, Y. Zhu, B. Li, and C.-L. Huang, A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 2020: p. 1-4.
- Brodin, P., Why is COVID-19 so mild in children? Acta Paediatrica. n/a(n/a).
- Bunyavanich, S., A. Do, and A. Vicencio, Nasal Gene Expression of Angiotensin-Converting Enzyme 2 in Children and Adults. JAMA, 2020. 323(23): p. 2427-2429.
- Patel, A.B. and A. Verma, COVID-19 and Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: What Is the Evidence? JAMA, 2020.
- Miller, A., M.J. Reandelar, K. Fasciglione, V. Roumenova, Y. Li, and G.H. Otazu, Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. medRxiv, 2020: p. 2020.03.24.20042937.
- Sidiq, K.R., D.K. Sabir, S.M. Ali, and R. Kodzius, Does Early Childhood Vaccination Protect Against COVID-19? Frontiers in Molecular Biosciences, 2020. 7(120).
- World Health Organization (WHO), Global Routine Immunization Strategies and Practices (GRISP): a companion document to the Global Vaccine Action Plan (GVAP). 2016.
- Dai, B., Z.H. Chen, Q.C. Liu, T. Wu, C.Y. Guo, X.Z. Wang, H.H. Fang, and Y.Z. Xiang, Duration of immunity following immunization with live measles vaccine: 15 years of observation in Zhejiang Province, China. Bulletin of the World Health Organization, 1991. 69(4): p. 415-423.
- Medina, R.A., B. Manicassamy, S. Stertz, C.W. Seibert, R. Hai, R.B. Belshe, S.E. Frey, C.F. Basler, P. Palese, and A. García-Sastre, Pandemic 2009 H1N1 vaccine protects against 1918 Spanish influenza virus. Nature communications, 2010. 1(1): p. 1-6.
- Lee, P.-I., Y.-L. Hu, P.-Y. Chen, Y.-C. Huang, and P.-R. Hsueh, Are children less susceptible to COVID-19? Journal of Microbiology, Immunology, and Infection, 2020.
- Lee, J., Mental health effects of school closures during COVID-19. The Lancet Child & Adolescent Health, 2020. 4(6): p. 421.
- Centers for Disease Control and Prevention (CDC). Keep Children Healthy during the COVID-19 Outbreak (https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/children.html ) Accessed on 1/6/2020. 2020
- World Health Organization (WHO). Coronavirus disease (COVID-19) advice for the public: Advocacy (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/healthy-parenting) (Accessed on 5/6/2020). 2020
